Goals & Recommendations
BACKGROUND: The Centers for Medicare & Medicaid Services (CMS), which oversees the Medicare program, contracts with 18 End Stage Renal Disease (ESRD) Network Organizations throughout the United States to perform oversight activities to ensure appropriateness of services and protection for ESRD patients. Quality Insights Renal Network 3 (QIRN 3) is the ESRD Network contractor selected to serve New Jersey, Puerto Rico and the US Virgin Islands.
REQUIRED NETWORK GOALS FOR ALL FACILITIES:
-
Participate in and meet deadlines for Network led-activities. Notify the ESRD Network of key personnel changes.
-
Access the Network ESRD Facility Dashboard and pursue achievement of the goals assigned for:
-
Increase Home Dialysis (Direct Starts and Transition from in-center)
-
Increase Transplant (Waiting list and Transplantation)
-
Increase Vaccinations (COVID: patients & staff, Influenza: patients & staff, Pneumococcal: patients)
-
Reduce Hospital Admissions, Readmissions, and Outpatient Emergency Visits
-
Increase Patient Engagement (Patient-to-Patient Support, Inclusion in QAPI meetings, use of a Life Plan to develop the patient’s plan of care)
-
Meet the CMS goals for Forms Reporting Deadlines (2728 within 45 days, 2746 within 14 days)
-
Establish and maintain a quality assessment and performance improvement program that evaluates the care provided and identifies opportunities for and continuously works to improve care delivered.
-
Centers for Medicare and Medicaid (CMS) End Stage Renal Disease (ESRD) Quality Incentive Program (QIP)
CfC Interpretative Guidelines, § 494.110 Condition: Quality assessment and performance improvement (V628) states, Where minimum outcome values have been determined, facilities are expected to provide care directed at achievement of at least the minimum outcome value by all patients.
Facilities that have achieved the minimum goals shall strive to meet or exceed the top 10% goals.
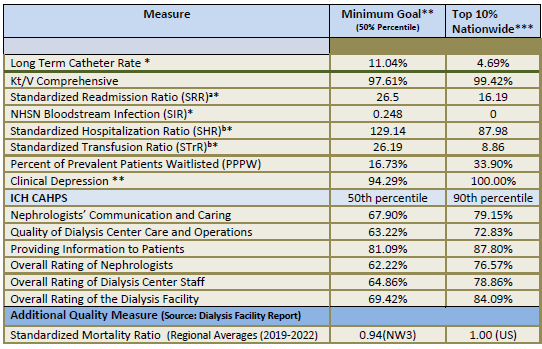 Source: Federal Register
Source: Federal Register
* On these measures, a lower rate indicates better performance.
**Minimum Goal- This is the CMS ESRD QIP Final PY 2026 Performance Standard, which is the 50th percentile of performance rates nationally Data sources: VAT measure: 2022 EQRS; SRR, SHR: 2022 Medicare claims; STrR: 2022 Medicare claims; Kt/V:
2022 EQRS; Hypercalcemia: 2022 EQRS; NHSN: 2022 CDC; ICH CAHPS: CMS 2022; PPPW: 2022 EQRS and
2022 Organ Procurement and Transplantation Network (OPTN); Clinical Depression: 2022 EQRS.
***Top 10% Nationwide- This is the CMS ESRD QIP Final PY 2026 Benchmark, which is the 90th percentile (Best 10% of units) of performance rates nationally during CY 2022. Facilities that meet or exceed these rates will likely earn the full points for the specified measure.
ᵃ Rate calculated as a percentage of hospital discharges. ᵇ Rate per 100 patient-years.
RECOMMENDATIONS FOR ALL FACILITIES:
Adequacy
-
Residual renal function should be incorporated into adequacy measures when appropriate
Data and Reporting Systems
-
Submit data and information timely and accurately as defined by project to the Network and in End Stage Renal Disease Quality Reporting System (EQRS) as is required by law and regulation.
-
Register in NHSN, enroll in the Network 3 group and submit dialysis event data and information timely and accurately on a monthly basis.
Emergency Preparedness
-
NJ facilities- Report reportable events including emergencies that disrupt dialysis delivery through NoviSurvey. For guidance on how to report in NoviSurvey, email NonLTC.Reportables@doh.nj.gov.
-
Designate two disaster representatives for the facility and provide alternate contact information in EQRS for primary and secondary disaster personnel.
-
Notify the Network if the facility activates its contingency plans due to an emergency event, facility plans to close or alter treatments and/or there is impact to facility operations. Link: https://esrdqiaforms.qualityinsights.org/nw3/emergencyevent/create
Health Equity
-
Adopt relevant social and structural determinants of health (SDOH) screening tools.
-
Make use of Network tools and training—video-based microlearns, technical assistance, tip sheets—to appropriately screening for, collecting, and reporting SDOH data.
-
Promote language equity and inclusivity by:
-
Implementing a Culturally and Linguistically Appropriate Services (CLAS) Action Plan
-
Providing health literate patient and family materials
-
Modality Education
-
Assess and refer in a timely manner medically suitable patients to treatment modalities that increase rehabilitation and independence including in-center self-care, home self-care and transplantation.
-
NJ specific- NJ state regulations require a transplant surgeon or designee is a part of the plan of care interdisciplinary team. (N.J.A.C Title 8 Chapter 43 8:43A-24.13 Patient care plan).
Patient Experience of Care
-
Clearly delineate and respect the rights and responsibilities of both the patient, family, significant others and the facility while promoting patient/family centered care and engagement.
-
Actively consult with the Network regarding difficult patient situations prior to any situation escalating to the consideration of an involuntary discharge.
-
Promote patient-appropriate access to in-center dialysis care at the facility level by:
-
Avoiding involuntary discharges (IVDs) and involuntary transfers (IVTs)
-
Assisting in the placement of patients at risk for IVDs or IVTs
-
Patient Education
-
Make available to patients Network-provided information on its Quality Improvement Projects, the CMS ESRD QIP, Regional and National profiles of care, the importance of immunization, information on how to access and use CMS Dialysis Facility Compare.
-
Educate patients about all treatment options at initiation of renal replacement therapy annually, and at additional times if indicated by changes in clinical condition.
Patient Engagement
-
Welcome, seek and respect the involvement of the patient, including their family as requested, in every aspect of medical care.
-
Patients should be provided the opportunity to define the members of their families.
-
Work to increase the number of patients participating in their care planning.
-
Encourage patients to become Network subject matter experts to provide the patient perspective in quality improvement activities.
Patient Safety
-
All facilities are urged to embrace a “culture of safety” and initiate specific measures to enhance safety, and prevent/reduce medical errors, such as:
-
Use a standardized abbreviation list
-
Use stickers to warn of allergies, of like or similar names and anticoagulation therapy
-
Post a list of drug dialyze‐ability, or drugs to avoid during dialysis
-
Track adverse events/incidents
-
Identify and track healthcare‐associated infections (HAIs) that develop during the course of care in the facility, and report such infections in NHSN
-
Identify, track and use preventative measures against central line‐associated blood stream infections (CLABSIs) that include:
-
Routine review of central venous line care procedures with healthcare workers and patients
-
Removal of non‐essential central venous lines
-
-
-
All facilities are encouraged to participate in the Quality Insights' 5‐Diamond Patient Safety Program
-
Follow the CDC’s Recommendations for Preventing Transmission of Infections Among Chronic Hemodialysis Patients.
Appendix 1 and 2 - Download Printable Version
Resources
-
Fact Sheet: CY 2024 ESRD PPS Final Rule Fact Sheet | CMS
-
PY 2026 Final Rule: https://public-inspection.federalregister.gov/2023-23915.pdf
-
CY 2024 Technical Specifications: https://www.cms.gov/files/document/cy-2024-proposed-technical-specifications-20230630.pdf
-
KDOQI Guidelines: https://www.kidney.org/professionals/guidelines
-
NHSN CDC Dialysis Component: https://www.cdc.gov/nhsn/dialysis/event/index.html
-
Dialysis Facility Report: https://dialysisdata.org/
MRB approved: 02/23/2024

